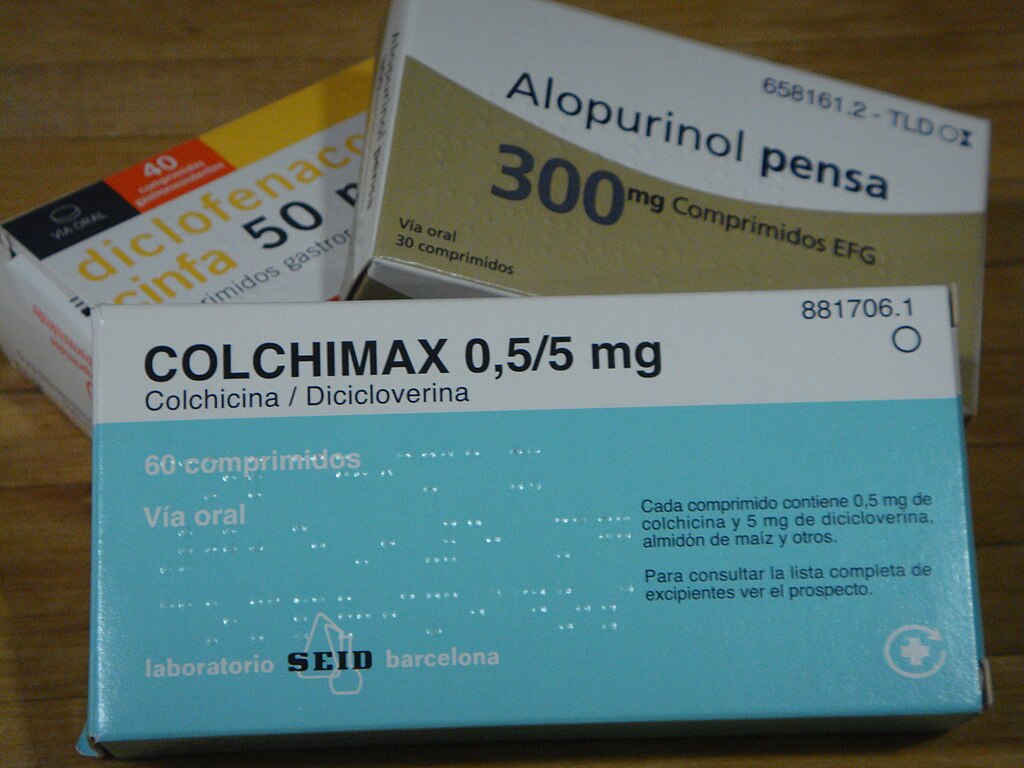
Colchicine use reduces strokes and heart attacks in people with cardiovascular disease, according to a Cochrane review
A review conducted by the Cochrane Collaboration analyzed the effects of colchicine—a medication commonly used to treat some rheumatic diseases—on people who had already experienced a cardiovascular event. The review included 12 clinical trials with more than 23,000 patients and concluded that colchicine reduces the risk of stroke or heart attack in these individuals. Overall, for every 1,000 people treated, there were 9 fewer heart attacks and 8 fewer strokes compared to those who did not take the medication, with no apparent serious side effects.
Sendón - Colchicina (EN)
José Luis López Sendón
Cardiologist at La Paz Hospital and researcher at IdiPAZ (Madrid)
This is a detailed review of studies analyzing the effect of colchicine versus placebo in patients with cardiovascular disease. It is not the first meta-analysis on this topic, but Cochrane reviews are renowned for their quality and impartiality, making them a valuable resource for scientists, drug regulatory agencies, and physicians in general.
Several recent meta-analyses have addressed this topic—the usefulness of low-dose colchicine in secondary prevention of cardiovascular disease—and this one corroborates previous findings: in secondary prevention of cardiovascular disease, administering low-dose colchicine reduces myocardial infarction and stroke compared to control groups receiving a placebo. No increase in adverse effects was observed. It was not shown to reduce mortality, which diminishes the significance of the results.
What this review brings to the table is the reliability of the data analysis using Cochrane methods. It does not offer any novel conclusions and I believe it will have few implications. Its greatest asset is the Cochrane Review's prestige.
[Regarding potential limitations] The reasons why some studies yielded good results and others did not are not discussed. Furthermore, there are three limitations I would like to point out:
Complexity of the inflammatory process. The benefit of colchicine in this population is attributed primarily to its anti-inflammatory effect. It is well established that inflammation, associated with virtually any cardiovascular risk factor and any infection such as the flu, poor dental health, and others, has a direct impact on the progression of atherosclerosis and cardiovascular disease. However, studies with different anti-inflammatory drugs for cardiovascular prevention have yielded negative results or unacceptable side effects, except for colchicine.
Dosage. In all studies, colchicine was administered at a fixed dose throughout the study's observation period. It is highly likely that over several months, the degree of inflammation will vary, with periods of very low or very high inflammatory activity. We need new studies that consider patient selection and dose adjustment according to the degree of inflammation at any given time.
Funding difficulties. Colchicine is the Cinderella of the anti-inflammatory world: it has proven efficacy and potentially better results, but lacks resources for research and promotion of its use. The future of research in this field currently rests in the hands of a relatively small group of scientists who do not give up in the face of difficulties. And they need public funding to continue their research.
Ana Viana - colchicina
Ana Viana Tejedor
Acute Cardiac Care Unit Coordinator. Cardiovascular Institute. Hospital Clínico San Carlos. Madrid; Associate Professor of Medicine at Complutense University of Madrid; and President of the Association of Ischemic Heart Disease and Acute Cardiac Care of the Spanish Society of Cardiology
The article is of high quality. It belongs to the Cochrane Collaboration, which means that it has a rigorous and reproducible design, with a previously registered protocol. The inclusion criteria are strict, only including randomized clinical trials with ≥6 months of follow-up and an independent, double assessment of risk of bias (RoB2). A comprehensive review of sources (CENTRAL, MEDLINE, EMBASE, FDA, etc.) has been carried out up to February 2025, making it very up-to-date. There are no indications of serious bias or relevant conflicts of interest.
Therefore, in terms of rigor, it is a very comprehensive and methodologically sound review of colchicine in secondary cardiovascular prevention.
The review does not revolutionize knowledge, but it definitively consolidates the evidence accumulated since 2019 (COLCOT, LoDoCo2, CLEAR-SYNTAX trials, etc.) showing that:
- Colchicine consistently reduces the risk of myocardial infarction and stroke (≈25–30% relative reduction).
- It does not alter total or cardiovascular mortality.
- It does not increase serious adverse events, although it does increase mild gastrointestinal effects.
New features and added value:
- It integrates 12 randomized clinical trials and nearly 23,000 patients, doubling the sample size compared to previous meta-analyses.
- It updates the evidence by including the most recent trials (2023–2024).
- It reinforces the benefit in myocardial infarction and stroke with “high-certainty evidence” (according to GRADE).
- It provides a neutral synthesis with no apparent publication bias, something that some previous meta-analyses could not guarantee.
How it fits into current guidelines:
- It confirms and strengthens the recommendation already present in the 2024 ESC European guidelines on chronic coronary syndrome, where colchicine (0.5 mg/day) is a class IIa indication in patients with stable atherosclerotic disease despite optimal treatment.
- It helps consolidate its role as a low-cost, well-tolerated cardiovascular anti-inflammatory.
Implications:
- Clinically, this meta-analysis reinforces colchicine as a safe, inexpensive, and effective tool in secondary prevention, especially in patients with recurrence or persistent inflammation.
- Next steps:
- Better define which subgroups (e.g., by inflammation biomarkers) benefit most.
- Evaluate long-term effects on mortality and quality of life.
- Analyze implementation in real practice (adherence, cost-effectiveness, interactions).
Although robust, the review has some important limitations:
- Indirect evidence on mortality: trials were not designed to detect changes in mortality; follow-up periods (6–80 months, median ~2 years) are relatively short.
- High heterogeneity in gastrointestinal events, indicating variability between studies and making it difficult to quantify risk accurately.
- Selected populations: Most participants were men (≈80%) with stable ischemic heart disease; extrapolation to women, elderly patients, or patients with heart failure is uncertain.
- Lack of data on quality of life and hospitalizations, which are relevant outcomes for clinical practice.
- No subgroup analysis according to residual inflammation (e.g., hsCRP levels). This limits understanding of who benefits most (possibly those with persistent inflammation).
- Treatment duration and adherence: Most trials used colchicine for 1–3 years; its long-term efficacy and safety (>5 years) remain unclear.
Pascual - Colchicina (EN)
Domingo Pascual Figal
Head of the Cardiology Department at the Virgen de la Arrixaca Hospital and Professor at the University of Murcia
This work is necessary precisely because it is a high-quality meta-analysis, endorsed by Cochrane, at a time when sufficient clinical trials exist to establish a solid and critical level of evidence on the value of colchicine as an anti-inflammatory drug in cardiovascular disease.
While clinical trials exist, the results have shown some heterogeneity. Overall, the results have been favorable, and American guidelines have recommended low-dose colchicine in patients with high cardiovascular risk to a greater degree than European guidelines, which recommend it less strongly. In this context, this extensive, high-quality meta-analysis provides new evidence, as it combines the information from all these individual trials and translates it into a comprehensive view of the drug's benefits and adverse effects within the broader context of cardiovascular, coronary, and cerebrovascular disease.
The main limitation is inherent to the individual trials themselves: the benefit is moderate and predominant in patients with ischemic heart disease (previous myocardial infarction), but we likely lack data on which subgroups of patients may benefit most. In particular, colchicine is an anti-inflammatory drug, and it would be relevant to identify markers that would help to individualize or personalize this treatment in those patients in whom this mechanism is predominant in their cardiovascular risk.
Ebrahimi et al.
- Research article
- Review
- Peer reviewed
- People



