Clínic Hospital
If you are the contact person for this centre and you wish to make any changes, please contact us.
Head of the Cardiology Department at the Hospital Clínic de Barcelona and researcher at the National Centre for Cardiovascular Research (CNIC) and at the August Pi Sunyer Biomedical Research Institute (IDIBAPS)
Neurologist at the Hospital Clínic in Barcelona
Head of Microbiology at Hospital Clínic in Barcelona, associate professor at the University of Barcelona, and researcher at ISGlobal Barcelona
Psychiatrist and researcher at the Bipolar and Depressive Disorders Unit of the Hospital Clínic de Barcelona
Head of the Arrhythmias and Physical Activity research group at IDIBAPS, cardiac electrophysiologist at Hospital Clínic Barcelona, associate professor of Medicine at the University of Barcelona and researcher at CIBERCV.
Professor of Psychiatry at the University of Barcelona, Head of the Psychiatry and Psychology Department at Hospital Clínic in Barcelona, and researcher at the Biomedical Research Centre in Mental Health (CIBERSAM)
Psychiatrist and researcher at the Depressive and Bipolar Disorders Unit of the Hospital Clínic de Barcelona
Assistant Doctor of Psychiatry and postdoctoral researcher at the Bipolar and Depressive Disorders Unit of the Psychiatry and Psychology Department of the Hospital Clínic de Barcelona.
Professor of Medicine at the University of Barcelona and coordinator of the Central Sensitisation Unit at the Hospital Clínic de Barcelona.
Research Professor at IDIBAPS-Hospital Clínic de Barcelona and Scientific Director of CIBEREHD - Carlos III Health Institute

Exposure to cold and heat could affect adolescents' mental health, according to a study published in JAMA Network Open. The research, led by the Barcelona Institute for Global Health (ISGlobal), was conducted with nearly 5,000 adolescents from the Netherlands (3,934) and Spain (885). The results showed how exposure to environmental temperatures influences psychiatric symptoms such as anxiety, depression, and attention problems.
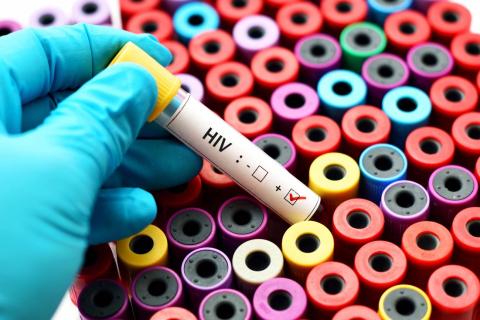
Science magazine has named lenacapavir as breakthrough of the year. Lenacapavir is an injectable drug that prevents HIV infection for six months with near 100% efficacy. The publication notes its potential to dramatically reduce infections in high-risk populations, but also reminds that global roll-out will depend on affordability, manufacturing agreements and a robust health infrastructure. Approval of the drug is expected by 2025.
CAR-T cell-based treatments have been successful against some blood tumours, but are much less effective for solid tumours. A phase 1 clinical trial has tested their use in 11 children and young adults with diffuse midline glioma, a tumour of the nervous system that is considered incurable. The results, published in the journal Nature, indicate that the treatment improved functional status in nine of the 11 patients. One of the four who showed a strong response is still healthy four years later.

The U.S. FDA has approved a new drug—called Cobenfy—to treat the symptoms of schizophrenia. Unlike traditional treatments, which are based on blocking the effects of dopamine, its mechanism of action simulates the effects of another neurotransmitter, acetylcholine. It is the first drug to be approved with a different mechanism of action in over 70 years.

The regulatory agencies for medicines in the United States and Europe have issued statements informing about a possible risk of developing certain types of tumors following CAR-T cell immunotherapy treatment. What do we know so far? What is the real risk? Does the benefit-risk balance still hold? Has anything changed after these alerts? We answer these questions with expert opinions and the data currently available.

Five out of ten potential treatments move from animal studies to human studies; four to randomised controlled clinical trials; and one in 20 moves on to approval by regulatory agencies, an analysis estimates. Concordance between positive results in animals and in clinical studies is 86%, according to the study, published in PLoS Biology, which pools the findings of 122 published studies on 54 different human diseases.

CAR-T cell therapies may, in some cases, produce tumours secondary to treatment. A few months ago, the US Food and Drug Administration (FDA) said it was assessing this risk. Now, a study conducted at Stanford University Medical Center (USA) has tracked 724 patients who received this type of treatment since 2016. Of these, 14 developed another blood tumour, but only one was a T-cell lymphoma that could be a direct consequence of the therapy. Further analysis ruled out this link. The results are published in the journal NEJM.

The Lancet Psychiatry publishes the first meta-analysis of the incidence of antidepressant treatment discontinuation symptoms that includes data from more than 20,000 patients collected from 79 randomised controlled trials and observational studies. The study sought to distinguish between symptoms directly caused by medication discontinuation and other ‘non-specific’ symptoms that may be associated with patient or professional expectations (the nocebo effect). The study concludes that one in six to seven patients will experience one or more symptoms directly caused by stopping medication, and one in 35 are likely to experience severe symptoms.
The Science group is simultaneously publishing four papers (two in the journal Science, one in Science Immunology and one in Science Translational Medicine) that include advances in a sequential vaccination strategy for an effective HIV vaccine. The methods employed aim to obtain broad-spectrum neutralising antibodies and one of the proposals is already in clinical trials.

The largest meta-analysis to date that studies the risk of children of people with a mental disorder also suffering from some type of mental disorder during their lifetime has been published, with Spanish participation. According to the study, the risk is more than double that of the rest of the population. To explain the study and resolve any doubts that may arise, the Science Media Centre Spain organised an information session with one of the authors, psychiatrist Joaquim Raduà.