A study links the development of lupus to the Epstein-Barr virus
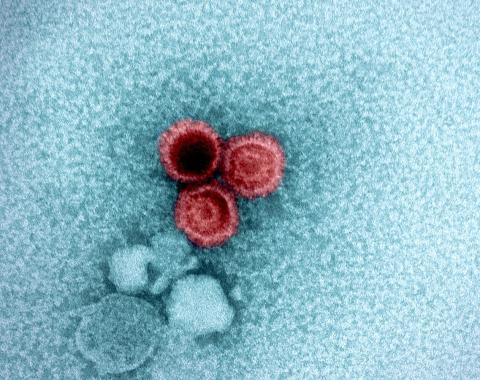
The Epstein-Barr virus, which causes mononucleosis, or the kissing disease, is present in approximately 95% of adults. Recent studies have confirmed its link to the vast majority of multiple sclerosis cases. Now, a US team has uncovered a mechanism that would also establish its connection to the development of systemic lupus erythematosus. “We believe it applies to 100% of cases of the disease,” the authors state, publishing their results in the journal Science Translational Medicine.
Cervera - Lupus EN)
Ricard Cervera
Rheumatologist and Head of the Autoimmune Diseases Service at Hospital Clínic de Barcelona
This is a high-quality, original article that convincingly demonstrates the pathogenic role of Epstein-Barr virus infection in systemic lupus erythematosus.
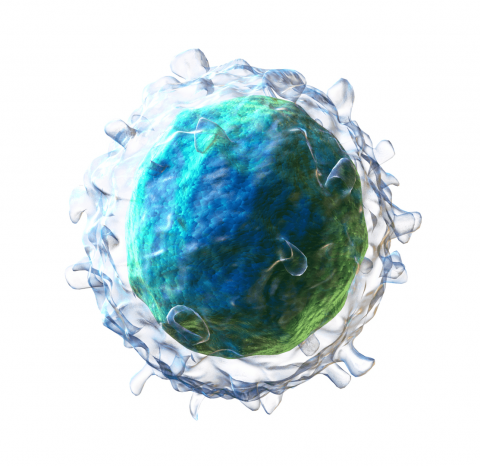
For more than 50 years, this and other viruses have been postulated as pathogenic in systemic lupus erythematosus and other autoimmune diseases; however, this is the first study to conclusively demonstrate the mechanism by which Epstein-Barr virus causes alterations in B lymphocytes that lead to the development of autoimmunity.
Although latent Epstein-Barr virus is present in most adults, it resides in only a small fraction of any individual's B lymphocytes. Until this study, it was virtually impossible to identify infected B lymphocytes and distinguish them from uninfected ones. In this study, using a highly accurate sequencing system, the authors discovered that fewer than 1 in 10,000 B lymphocytes in a typical, otherwise healthy individual infected with the Epstein-Barr virus harbor a latent viral genome. In contrast, in patients with lupus, the proportion of B lymphocytes infected by this virus increases to approximately 1 in 400.
This latent virus, despite its near-total inactivity, incites B lymphocytes to produce a viral protein, EBNA2. The researchers demonstrate in this study that this protein acts as a “transcription factor” (similar to a molecular switch) that activates a series of B lymphocyte genes, which encode proteins that, in turn, are transcription factors that activate various pro-inflammatory human genes. The ultimate consequence of all this genetic interaction is that B lymphocytes become highly inflammatory, transforming into “antigen-presenting cells” and beginning to stimulate other immune cells (helper T lymphocytes) that share the predilection for attacking nuclear components. These helper T lymphocytes recruit a multitude of other B lymphocytes, as well as killer T lymphocytes, which are ferocious attackers of the immune system.
This would imply that a more aggressive treatment against the Epstein-Barr virus in these patients with a higher proportion of infected B lymphocytes could slow down or, ideally, cure the disease.
The main limitation of this work is the small number of patients in whom this study was conducted, which necessitates replicating it in larger cohorts with different clinical variants of this disease
Younis et al.
- Research article
- Peer reviewed
- People